Psychedelic-Assisted Psychotherapies: A Policy Perspective with Victor Cabral – PESI
69,00 $ Original price was: 69,00 $.15,00 $Current price is: 15,00 $.
You may check content proof of “Psychedelic-Assisted Psychotherapies: A Policy Perspective with Victor Cabral – PESI” below:
Psychedelic-assisted psychotherapy: a policy viewpoint
In recent years, the study of psychedelic-assisted psychotherapies has received extraordinary interest, both in clinical settings and in the larger public debate around mental health care. After decades of stigma and restriction due to government drug policy, drugs such as psilocybin and MDMA are finally being acknowledged for their potential therapeutic advantages in the treatment of a variety of mental health disorders, including depression, PTSD, and anxiety. This transition represents a paradigm shift, requiring not just cautious regulation but also ethical concerns and public discussion. Psychedelic treatments have the potential to alter mental health care, sparking vital conversations among politicians, healthcare practitioners, and the general public.
Psychedelic-assisted therapies are at the confluence of science, culture, and ethics. Many psychologists and academics now consider them as possible lifesavers, having previously been viewed as harmful and entirely recreational substances. However, the road ahead is laden with complications as the regulatory structure controlling these compounds matures. This post will look at the complex relationship between legislation, cultural attitudes, and ethical practice in the context of psychedelic-assisted treatments. The paper will carefully examine pathways for integration within current health systems while addressing inequities in access and equality.
Regulatory Framework
The regulatory environment for psychedelic-assisted psychotherapies has undergone substantial change in response to increased research and public interest. Many psychedelics, including psilocybin and MDMA, are now listed as Schedule I drugs under the Controlled drugs Act, indicating that they have a high potential for abuse and no accepted medicinal value. This categorization introduces hurdles to research and clinical practice, potentially impeding the development of these promising medicines. However, recent developments show a readiness at both the federal and state levels to consider legal amendments targeted at increasing access to psychedelics for therapeutic purposes.
Legislation affecting psychoactive treatments
Legislative changes are critical in determining the environment for psychedelic therapy. Various states have taken steps to legalize or control the use of psychedelics, demonstrating the trajectory of this development. For example, in 2020, Oregon passed Measure 109, which provides for a controlled psilocybin therapy program. Oregon’s legislation exhibits a progressive approach to mental health treatment by establishing a framework that allows for the supervised administration of psilocybin.
Similarly, Colorado’s 2022 initiative to legalize the therapeutic use of psychedelics is another watershed moment, indicating the public’s readiness to accept these drugs in health-care settings. These legislative initiatives serve as a barometer for altering public perception about psychedelics’ therapeutic benefits, opening the door for further study and clinical implementation. Furthermore, these developments have the potential to cause a nationwide ripple effect, prompting other states to reconsider their drug laws in light of increasing research and cultural views.
However, when state legislation advances, it frequently faces conflicts with federal restrictions. The conflict between state-led efforts and existing federal legislation provides a stumbling block for practitioners and researchers, raising concerns about the legality and acceptance of psychedelic treatments worldwide. Advocates are advocating for sweeping federal changes to decriminalize psychedelics, resulting in a unified framework that combines state initiatives with federal regulations.
State vs. federal regulations
In the context of psychedelic-assisted treatments, the interaction between state and federal rules is complicated and occasionally contradicting. Policy bifurcation creates an uncertain environment for both practitioners and patients. For example, while Oregon has created frameworks that allow for psilocybin therapy, the federal government continues to categorize it as a Schedule I substance, essentially making it illegal on the federal level. This juxtaposition creates a slew of obstacles for financing, research, and the practical implementation of psychedelic-assisted psychotherapies.
State-level initiatives frequently reflect a rising public interest and demand for the mental health options that psychedelics provide. Colorado and Oregon demonstrate how state governments may adopt proactive approaches to mental health, but ongoing federal constraints impede wider access and implementation. This mismatch might cause misunderstanding and worry among patients and healthcare professionals, reducing their desire to engage with various therapy options.
The ongoing debate over state vs federal rules is critical for creating a favorable climate for psychedelic-assisted treatments to thrive. Advocates say that more coordination between state and federal policies is required to support research, enhance public safety, and assure equal access to treatment choices. Moving forward, creating alignment between these regulatory frameworks will be critical to realize the full potential of psychedelic-assisted psychotherapies in the American healthcare system.
International Policy Trends
While the United States navigates its regulatory landscape, foreign patterns suggest a larger shift toward acceptance of psychedelic-assisted therapy. Countries such as Canada and Australia are establishing important examples for regulatory changes that acknowledge the medicinal potential of these drugs. In Canada, the Special Access Program has recently been expanded, giving more patients access to psychedelics for therapeutic use. Meanwhile, Australia has formally legalized psychedelic therapy, allowing physicians to prescribe MDMA and psilocybin for PTSD and treatment-resistant depression starting in February 2023.
Furthermore, other countries, such as Jamaica and the British Virgin Islands, have taken a more permissive approach to psychedelics, allowing the production and consumption of drugs such as psilocybin mushrooms. By establishing legal frameworks for these drugs, these nations are encouraging the development of a commercial psychedelics industry that promotes research and safe practices.
Globally, these developments indicate an emerging grasp of the harm-reduction potential that regulatory change might deliver. As the public’s interest in psychedelic medicines grows, the international community’s answers may enlighten and motivate US legislators to consider alternate legislative approaches. This changing landscape provides an opportunity not just for study but also for treating mental health crises through novel treatment approaches.
Ethical consideration
As psychedelic-assisted treatments gain popularity, ethical issues become increasingly important. Healthcare practitioners must traverse complicated ethical quandaries, particularly those involving informed consent, risk management, and cultural competency. As therapies utilizing chemicals capable of altering perceptions and consciousness gain momentum, the construction of a strong ethical framework is critical to guaranteeing patient safety and successful therapeutic procedures.
Informed consent for psychedelic treatment
Informed consent in psychedelic-assisted therapy poses unique issues when compared to regular mental health treatments. Psychedelics can substantially alter consciousness, thus patients must be well informed of the dangers and benefits of these therapies. It is critical for doctors to offer full explanations that include not just the therapy procedure and expected benefits, but also the possibility of severe psychological experiences and any negative consequences.
Practitioners should have detailed talks regarding the nature of psychedelics, the therapeutic environment, and the significance of post-session integration. Failure to appropriately educate patients may jeopardize the therapeutic experience and the treatment’s ethical integrity. Furthermore, practitioners should be acutely aware of the special vulnerabilities of patients seeking psychedelic treatments, particularly those from marginalized communities or those suffering from serious mental health difficulties.
The changing legal landscape around psychedelics hampers informed consent. As more governments embrace progressive regulations, the ethical criteria around consent must be clearly stated and universally applied. Practitioners must remain up to date on the growing legal and ethical implications of psychedelics in order to offer proper care that respects patient autonomy and optimizes therapeutic potential.
Balancing risks and advantages.
Both practitioners and patients must strike a balance between dangers and benefits while using psychedelics. While psychedelics have the ability to alter lives, the hazards connected with their usage must not be underestimated. Patients must be informed not just of the treatment’s immediate effects, but also of any potential long-term consequences.
Continuous monitoring of patients during and after psychedelic sessions is critical to assuring safety and efficacy. Establishing guidelines for analyzing patient reactions might aid in managing any side effects that may emerge throughout the therapy process. Furthermore, it creates a supportive and comfortable environment for patients, allowing them to manage their experiences without fear or worry.
Cultural competency is also an important consideration in risk-benefit analyses. Clinicians must understand how cultural backgrounds shape conceptions of mental health and recovery procedures. Practitioners can improve therapeutic outcomes by using culturally relevant approaches and being sensitive to their clients’ values. Furthermore, ensuring that therapies are available to a varied population helps to reduce inequities by establishing a sense of inclusion and understanding within the therapeutic setting.
Finally, the approach to psychedelic medicines must be based on ethical standards that promote patient safety and well-being. Healthcare practitioners may provide a therapeutic atmosphere based on trust and healing by carefully balancing the advantages and hazards and keeping attentive to cultural differences.
Cultural competency in treatment techniques.
Cultural competency is essential in the implementation of psychedelic-assisted treatments since patients’ different cultural backgrounds must be considered throughout the therapy process. Clinicians should aim to modify therapy approaches to reflect the values, beliefs, and experiences of people from other cultures. This adaptable approach not only helps to establish trust and rapport with clients, but it also promotes a supportive therapeutic atmosphere in which clients feel understood and valued.
Different cultures have distinct views on mental health, spirituality, and therapeutic traditions. More than ever, practitioners must connect with and learn from diverse viewpoints. Therapists can help clients process their experiences in a way that is meaningful to their identity by adding cultural narratives into the therapeutic journey. This can result in more effective outcomes and a reduction in feelings of alienation caused by culturally insensitive treatment approaches.
Cultural competency is also taken into account while recruiting various groups for clinical trials and therapeutic programs. Historically, racially and ethnically diverse people have been underrepresented in psychedelic research. Increasing study variety not only increases the scientific base of psychedelic-assisted treatments, but also guarantees that treatment techniques are relevant and reflective of the communities served.
Advocating for cultural competency in psychedelic-assisted treatments includes being self-reflective and questioning one’s own prejudices. Continuous self-assessment and training can help practitioners become more conscious of their cultural settings and assumptions, improving the therapeutic connection. To summarize, cultural competency is critical for developing an inclusive, respectful, and successful context in which psychedelic-assisted treatments can thrive.
Access and Equity
The growing interest in psychedelic-assisted therapy raises serious questions about equality and inequities among communities. As these new therapies become more widely accepted, policymakers and healthcare systems must emphasize equitable access to guarantee that all people may benefit from psychedelics’ therapeutic potential.
disparities in access to treatment
Disparities in access to psychedelic-assisted treatments highlight fundamental socioeconomic and racial disparities that now restrict the potential advantages for many people. Historically marginalized groups frequently encounter challenges to getting healthcare, such as a lack of information, financial constraints, and systematic prejudices within healthcare institutions. These obstacles can greatly limit the capacity of different groups to get potentially life-changing therapies.
Furthermore, the area of psychedelic research has been chastised for its lack of diversity, with studies generally failing to recruit ethnically diverse subjects. This lack of representation may perpetuate health inequities, given the safety and efficacy of psychedelic-assisted treatments on many demographic groups are unknown. The lack of various perspectives in this discussion limits the ability of these treatments to be adjusted to meet the specific mental health requirements of different ethnic groupings.
Policymakers must approach the integration of psychedelic-assisted treatments with equality as their guiding concept. Ensuring that clinical trials include a varied range of participants is critical for collecting complete data on treatment outcomes across multiple demographics. Furthermore, outreach efforts to educate underprivileged populations about the benefits of psychedelic therapy can help eliminate stigma and encourage informed decision-making.
Economic repercussions for patients.
The economic ramifications of access to psychedelic-assisted therapy exacerbate the already convoluted picture. As new therapies become accessible, their cost must be addressed so that financial constraints do not prevent people from receiving the care they require. The expenditures of psychedelic-assisted treatments, which may involve therapy sessions, chemicals, and integrating support, may quickly add up, especially for disadvantaged areas.
Furthermore, questions about insurance coverage for psychedelic therapy are critical. Advocating for policies that include these therapies in health insurance plans can dramatically improve access for those looking for alternative mental health care. Ensuring that these therapies are covered by insurance might close huge access gaps, allowing a larger population to reap the potential advantages of psychedelic-assisted psychotherapy.
Understanding the overall economic impact of mental health issues on society is critical. Depression and PTSD have significant economic consequences, including lost productivity, higher healthcare expenses, and worse health outcomes. Investing in research and integrating psychedelic treatments might reduce some of the stresses on both people and society in the short and long term.
Finally, regulations and programs that include the economic consequences of psychedelic therapies are required to promote a fair and inclusive approach to mental health care, enabling equal access for all people, regardless of income level.
Strategies for enhancing inclusion.
Strategizing for greater inclusion in psychedelic-assisted treatments necessitates deliberate, multidimensional methods that stress diversity and accessibility. As the sector advances, many essential measures can help break down barriers and build a more equal framework for providing care.
- Community Outreach and Education: Creating focused outreach initiatives for marginalized groups can help raise knowledge and comprehension of psychedelic therapy. Educating people on the advantages, hazards, and therapy procedures can help them make more educated healthcare decisions.
- Culturally Relevant Practices: Clinicians should explore incorporating culturally appropriate practices and therapeutic paradigms into the delivery of psychedelic-assisted therapy. Emphasizing diversity through multiple techniques may make the atmosphere more friendly to clients from all backgrounds.
- Varied Clinical Trials: Actively recruiting a more varied participant pool for clinical trials can result in richer data and guarantee that treatment regimens address the needs and experiences of different communities. This variability can improve the efficacy and safety of psychedelic medicines.
- Insurance Advocacy: Advocacy efforts should focus on promoting insurance coverage for psychedelic-assisted treatments, which will reduce cost obstacles and increase access. Engaging with health insurance companies can help design complete policies that promote equal access.
- Training for Practitioners: Educating physicians on the value of inclusion and cultural competency will help them provide better treatment. Continuous training and seminars can help therapists manage cultural sensitivity and better grasp the requirements of varied communities.
By employing these tactics, the therapeutic environment for psychedelic-assisted treatment may be drastically altered, promoting inclusion and equity of access, eventually leading to better mental health outcomes for all groups.
Research and Evidence
A substantial corpus of research is required to understand the efficacy and safety of psychedelic-assisted psychotherapies. As interest in these approaches rises, gathering data can help educate clinical practices, guide regulatory choices, and change public opinion.
Clinical trials and evidence-base
Numerous clinical trials have focused on the therapeutic uses of psychedelics such as psilocybin and MDMA. These trials show encouraging results for those suffering from a variety of mental health disorders, such as depression, anxiety, and PTSD. For example, a seminal research published in Nature Medicine discovered that 67% of patients undergoing MDMA-assisted therapy no longer satisfied the diagnostic criteria for PTSD 18 weeks following treatment. Research indicates that psychedelic-assisted therapy can promote intense emotional involvement with traumatic memories while also fostering emotions of safety and openness. This allows patients to digest their experiences in a controlled setting, which increases the therapeutic effects.
Psychedelics have a wide range of effects on brain circuits, increasing neuroplasticity and emotional control, giving them a unique potential for treating mental health conditions. As more research are conducted, the evidence foundation for psychedelic-assisted psychotherapy grows, paving the door for widespread adoption within the healthcare system.
As regulatory authorities such as the FDA launch Breakthrough Therapy Designations for drugs such as MDMA and psilocybin, the impetus behind research suggests a bright future for these treatments. Creating reliable methods to assess the efficacy of psychedelic-assisted therapy will be critical for developing clinical procedures and increasing acceptability among healthcare practitioners.
Limitations of Current Research
Despite the positive results of previous investigations, limits remain in psychedelic-assisted research. Methodological discrepancies, limited sample numbers, and a lack of long-term follow-ups are among the most significant problems. Many studies do not fully describe the exact therapeutic strategies used in psychedelic sessions, resulting in diversity in treatment procedures and outcomes.
Furthermore, participant expectations might bias outcomes, making it difficult to evaluate the findings. The widespread recreational use of these compounds outside of controlled research raises ethical and safety problems, frequently clouding the public’s impression of their therapeutic value.
Despite the existing evidence indicating considerable advantages, many regulatory authorities are wary due to the perceived lack of available data. A more systematic and consistent approach to research is required to address the pressing issues of methodology, participant variety, and long-term efficacy, eventually increasing the credibility of psychedelic-assisted treatments.
Future research directions.
Looking ahead, numerous critical areas provide chances to further psychedelic-assisted psychotherapy research. It is vital to broaden the scope of clinical studies to include a variety of psychedelics for diverse mental health disorders. Identifying which chemicals produce the best benefits for a wide range of diseases, including PTSD, anxiety disorders, and depression, can help to improve treatment regimens.
Furthermore, researchers should investigate the complex interplay between psychological processes and neurobiological systems that underpin treatment results. A better knowledge of how psychedelics affect brain function and cognition during therapy may lead to more effective treatment frameworks and procedures.
Future studies should stress varied demographic representation, addressing minority underrepresentation in clinical research. This inclusion will lead to a better knowledge of how diverse people respond to psychedelic medicines, while also ensuring that treatment procedures are tailored to the cultural demands of different cultures.
Finally, the advancement of psychedelic-assisted research necessitates a steadfast dedication to methodological integrity, diversity, and multidisciplinary cooperation. By accepting these concepts, we may maximize the promise of psychedelic medicines in the future of mental health therapy.
Training and Practice Standards
As the field of psychedelic-assisted psychotherapy expands, it becomes critical to develop rigorous training and practice standards. This ensures that practitioners have the information and skills needed to provide these novel therapies in a safe and ethical manner.
Credentialing practitioners
Credentialing practitioners engaging in psychedelic-assisted treatments is an important step toward ensuring legitimacy and safety in the area. Enhanced training programs are emerging that focus on the complexities of delivering psychedelics in therapeutic settings. Licensing agencies and certifying organizations must work together to establish minimal competency standards for mental health practitioners who wish to engage in these practices.
Courses at the California Institute of Integral Studies and Columbia University stress not just the pharmacological information required to comprehend psychedelics, but also therapeutic strategies, ethical issues, and cultural competency. Such thorough training is necessary for enabling therapists to negotiate the difficulties of psychedelic-assisted therapies while maintaining the highest levels of patient care.
The quest for certification is also intended to address concerns about the administration and efficacy of psychedelic therapy. Registered practitioners will be held accountable for following strong ethical and professional requirements, promoting public trust and protecting patients’ interests.
Training programs and prerequisites.
Numerous training programs are being established to help practitioners of psychedelic-assisted psychotherapy. To enroll in each program, applicants must meet particular educational and professional prerequisites.
For example, the California Institute of Integral Studies provides a Certificate in Psychedelic-Assisted Therapies, which comprises over 150 hours of training that combines academic understanding with experiential learning. Meanwhile, Columbia University has integrated psychedelic therapy training into its Master of Social Work program, ensuring that aspiring therapists acquire both classroom and clinical experience.
Overall, candidates for these training programs are frequently required to have graduate degrees in health-related subjects, as well as applicable licenses and therapy experience. This helps to guarantee that only competent professionals administer psychedelic-assisted treatments, and that they have the tools they need to do so safely and efficiently.
Continuous Professional Development
Continuous professional development (CPD) is vital for being competent in the rapidly expanding area of psychedelic-assisted treatment. As research advances, practitioners must keep current on new results, safety standards, and developing best practices.
Training programs usually provide continuing education seminars, workshops, and advanced subject discussions to enhance continued learning. These chances are critical for therapists to improve their abilities and stay current on the newest evidence-based techniques in psychedelic-assisted therapy.
In addition to formal training, constant self-assessment and reflection help practitioners eliminate biases and strengthen therapeutic interactions with clients. A dedication to CPD means that therapists approach psychedelic-assisted therapies with an open mind and are willing to alter their methods in response to new discoveries.
Finally, the development of thorough training and practice guidelines for psychedelic-assisted psychotherapy is critical to promoting ethical, successful, and inclusive practices. The discipline can guarantee that practitioners are competent to accompany patients through transformational therapeutic journeys by stressing comprehensive education, accreditation, and ongoing professional development.
Public perception, stigma
The public’s attitude of psychedelic-assisted therapy is evolving, driven by past stigma and contemporary scientific advances. As these treatments become more widely recognized for their therapeutic value, addressing the persisting stigma associated with psychedelics is critical for developing community acceptance and support.
Media portrayals of psychedelic treatment
Media coverage has a huge impact on popular attitudes about psychedelic-assisted therapy. Historically, news and entertainment sources have concentrated on sensationalized depictions of drug usage, adding to the stigma associated with psychedelics. Such narratives frequently focus on the risks and harms of these medications, overshadowing the rising data supporting their therapeutic benefits.
However, as clinical research progresses and favorable results emerge from thorough investigations, media portrayals of psychedelic therapy begin to evolve. By showcasing success stories and encouraging discussions about mental health care, the media may help dispel damaging misconceptions and educate the public about the complexities of psychedelic-assisted therapy.
Moving forward, it is critical to promote a balanced narrative that includes both the possible hazards and advantages of psychedelic therapy when provided under controlled conditions. Engaging the media in responsible storytelling can lead to a more educated public conversation that improves perceptions and raises mental health awareness.
Addressing Misconceptions
To successfully dispel myths about psychedelic-assisted treatments, mental health activists and clinicians must prioritize education and awareness efforts. Many misunderstandings arise from historical ties with counterculture drug usage and sensationalized media representations, which distort public perception.
Highlighting the thorough data that supports psychedelic-assisted therapy can help to combat unfavorable preconceptions of these medications. Demonstrating their empirical usefulness in treating disorders like PTSD, anxiety, and depression might help alter perceptions in a more positive direction. Advocacy groups should concentrate on disseminating evidence-based information about the organized therapy procedures involved, emphasizing that these therapies take place in safe, supervised environments.
Storytelling may also play an important role in dispelling misunderstandings. Sharing firsthand stories from people who have benefitted from psychedelic-assisted therapy adds real-world context to the prospective advantages. Such initiatives not only de-stigmatize the use of psychedelics in treatment, but also provide hope to persons with mental health difficulties.
Advocacy for Mental Health Awareness
Advocating for mental health awareness is crucial for increasing acceptance of psychedelic-assisted therapy. Mental health organizations, practitioners, and activists must work together to spark a conversation about the transformational power of psychedelics in recovery. This might include initiatives to raise public awareness about mental health concerns and the potential role of psychedelics in resolving them.
Advocates can raise awareness of the advantages and safety of psychedelic-assisted treatments through social media, community gatherings, and educational seminars. Engaging stakeholders, such as healthcare professionals and lawmakers, helps to keep mental health a top priority in public debate.
It is critical to rally support for research funding and regulatory changes that will improve access to psychedelic medicines. Engaging communities in advocacy initiatives allows individuals to express their concerns, building a feeling of togetherness in addressing mental health issues.
Ultimately, raising mental health awareness and removing stigma will lead to broader acceptance of psychedelic-assisted therapy. Advocates can help to foster a more compassionate approach to mental health care by providing knowledgeable and supportive surroundings for those seeking assistance.
Integration with current healthcare systems
The integration of psychedelic-assisted treatments into current health systems provides a unique challenge in the changing landscape of mental health care. As these therapies become more widely recognized for their potential advantages, it is critical to establish paths that allow them to coexist with established therapy techniques.
Collaborations with traditional therapy.
Collaboration with traditional therapy techniques is critical to the effective integration of psychedelic-assisted treatments. By framing these interventions as adjuncts rather than alternatives for established therapies, healthcare practitioners may deliver comprehensive care that addresses a wide spectrum of mental health conditions.
By adding psychedelics into conventional clinical methods, therapists may provide patients with a comprehensive approach that includes both pharmacological and psychotherapeutic advantages. This collaborative approach focuses on improving therapeutic outcomes while also instilling a sense of safety in clients exploring new treatment options.
Clinicians must be trained to guarantee that they have the abilities needed to incorporate psychedelic therapies into established therapeutic frameworks. Collaboration among healthcare experts can help to develop best practices and recommendations, paving the way for effective treatment regimens.
Furthermore, healthcare institutions must conduct outreach initiatives to educate employees and the general public about the advantages and hazards of psychedelic-assisted treatments, creating a climate conducive to their acceptance and integration.
Policy proposals for integration.
Policy proposals are critical to easing the incorporation of psychedelic-assisted treatments into existing healthcare systems. Establishing strong clinical practice standards is critical to ensuring the safe and successful delivery of these treatments. Professional organizations, such as the American Psychological Association (APA) and the American Psychedelic Practitioners Association (APPA), should take the lead in developing these evidence-based recommendations to help practitioners.
Insurance coverage for psychedelic-assisted therapy is another critical component of integration. Stakeholders in the insurance industry must create clear policies that are consistent with advancing clinical recommendations and promote equal patient access. Financial constraints can worsen existing health inequities, thus resolving these concerns is critical to maximizing the advantages of various treatment options.
Furthermore, comprehensive assessment and monitoring systems should be implemented to measure patient outcomes and ensure safety standards are followed. Implementing Risk Evaluation and Mitigation Strategies (REMS) can provide extra controls that improve patient access while focusing on safety during treatment.
Potential hurdles to systemic transformation.
Despite the potential of psychedelic-assisted treatments, a number of impediments prevent their systemic integration. Stigmatization and public fear about psychedelics can lead to resistance among healthcare practitioners and lawmakers, raising questions about their role in mental health therapy.
Furthermore, governmental scrutiny surrounding the approval and monitoring of psychedelic drugs may impede deployment. A perceived absence of a thorough evidence foundation for these medicines may discourage investment and wider acceptability within existing healthcare institutions.
Training needs are another possible impediment. As practitioners enter the nascent profession of psychedelic-assisted therapy, there is an immediate need for significant resources and institutional support to help them learn and train.
Overall, overcoming these obstacles will be critical to establishing psychedelic-assisted treatments as realistic therapeutic choices within existing healthcare systems. By removing stigmas, campaigning for legislative reform, and funding practitioner training, the mental health landscape may expand to embrace these potentially revolutionary therapy methods.
To summarize, the path to universal acceptance and incorporation of psychedelic-assisted psychotherapies in mental health care requires navigating a complicated interaction of regulatory frameworks, cultural perspectives, ethical concerns, and equitable access. As continued research reveals the therapeutic potential of these compounds, purposeful measures to alleviate inequities, improve training, and promote public knowledge will be critical. Healthcare practitioners, researchers, and policymakers may work together to create a more inclusive, knowledgeable, and successful approach to mental health treatment. Finally, the emergence of psychedelic-assisted treatments has the potential to be a watershed event in the future of mental health therapy, providing newfound hope and healing to innumerable people who are struggling.
Frequently Asked Questions:
Business Model Innovation:
Embrace the concept of a legitimate business! Our strategy revolves around organizing group buys where participants collectively share the costs. The pooled funds are used to purchase popular courses, which we then offer to individuals with limited financial resources. While the authors of these courses might have concerns, our clients appreciate the affordability and accessibility we provide.
The Legal Landscape:
The legality of our activities is a gray area. Although we don’t have explicit permission from the course authors to resell the material, there’s a technical nuance involved. The course authors did not outline specific restrictions on resale when the courses were purchased. This legal nuance presents both an opportunity for us and a benefit for those seeking affordable access.
Quality Assurance: Addressing the Core Issue
When it comes to quality, purchasing a course directly from the sale page ensures that all materials and resources are identical to those obtained through traditional channels.
However, we set ourselves apart by offering more than just personal research and resale. It’s important to understand that we are not the official providers of these courses, which means that certain premium services are not included in our offering:
- There are no scheduled coaching calls or sessions with the author.
- Access to the author’s private Facebook group or web portal is not available.
- Membership in the author’s private forum is not included.
- There is no direct email support from the author or their team.
We operate independently with the aim of making courses more affordable by excluding the additional services offered through official channels. We greatly appreciate your understanding of our unique approach.
Be the first to review “Psychedelic-Assisted Psychotherapies: A Policy Perspective with Victor Cabral – PESI” Cancel reply
You must be logged in to post a review.
Related products
Health
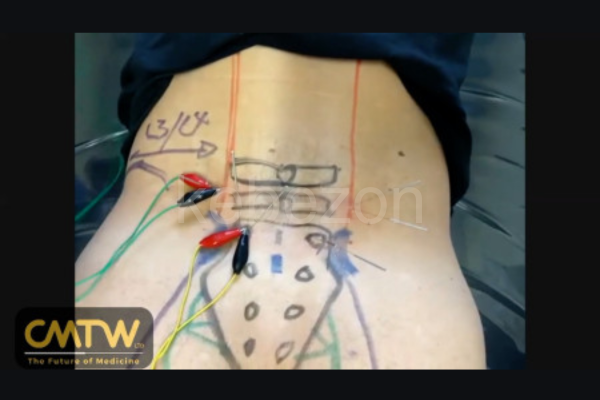
Assessment & Treatment of Lumbar Spinal Stenosis Using Electro-Acupuncture – Anthony Lombardi







Reviews
There are no reviews yet.